What every performance professional needs to know about tendon pain, pathology, and programming
Tendons are strong, collagen-rich tissues that connect muscle to bone, enabling efficient force transmission and movement.
They’re built to handle tension, and like springs, they store and release energy to enhance athletic performance.
But here’s the problem: tendons are also vulnerable.
When exposed to too much load too soon, they can’t keep up. That leads to degeneration, dysfunction, and pain.
Most tendon injuries follow a classic healing sequence:
- Inflammation
- Proliferation
- Remodeling.
Yet, in many athletes, the healing process stalls, mainly when rest and anti-inflammatory medications are prescribed as the go-to solution.
What is Tendinopathy?
Historically, tendon pain was labeled tendonitis, implying that inflammation was the primary driver.
However, research over the past two decades reveals a different story: most cases are degenerative, characterized by collagen breakdown, disorganized structure, and even the ingrowth of blood vessels, rather than inflammation.
That’s why we now use the broader term tendinopathy, which includes:
- Tendinosis: chronic degeneration without inflammation
- Tendonitis: rare, actual inflammation (typically acute overload)
The name matters because it shapes treatment.
And when we treat a degenerative tendon as if it were inflamed, we set recovery back, not forward.
The Problem with “Tendonitis” Treatments
Old-school treatments (e.g., NSAIDs, rest, cortisone shots) are still common. They might reduce pain in the short term, but they fail to promote healing.
In fact, research shows these interventions can delay tendon remodeling and may even weaken tissue over time.
The root issue in tendinopathy isn’t swelling, it’s tissue capacity vs. load.
When the load exceeds what the tendon can tolerate, structural degeneration begins. And unless we reintroduce the right kind of mechanical loading, that tendon won’t adapt or heal.
This message is at the heart of a new paper by Williams and Gyer (2025), published in the Journal of Musculoskeletal Surgery and Research (1).
Their commentary, Tendons Under Load: Understanding Pathology and Progression, synthesizes the current science and drives one key point home:
Tendons need load, not rest.
Let’s break it all down: what works, how tendon rehab should progress, and how coaches and clinicians can start applying this today.
Buckle Up.
The Progression of Tendinopathy
Rather than viewing tendon injury as binary (healthy or torn), the Continuum Model by Cook and Purdam, which this paper highlights, maps tendinopathy across three phases:
- Reactive Tendinopathy
- Acute overload causes swelling and thickening
- Matrix changes, not inflammation
- Can fully recover with proper load management
- Tendon Disrepair
- Collagen begins to separate
- Matrix becomes disorganized
- Partially reversible with smart rehab
- Degenerative Tendinopathy
- Cell death, acellularity, and major disorganization
- Rehab now focuses on function, not fixing the degenerated tissue
This continuum shifts the focus from “fix the tear” to “train the tissue.”
Even pathological tendons often have viable, loadable regions.
As Docking and Cook (2015) highlighted, we should focus on treating the “doughnut” – the healthy tissue – rather than the “hole” – the damaged area. This approach supports the idea that even in the presence of pathology, tendons can still be loaded effectively to promote adaptation and healing, especially when focusing on stimulating the healthy regions of the tendon.
Load Is the Medicine
Mechanical loading isn't just safe for tendons, it’s the primary driver of tendon adaptation.
Studies show that tendons adapt when exposed to:
- Progressive mechanical tension
- Heavy resistance training (70–85% 1RM)
- Specific patterns of isometric, isotonic, and eccentric movement
Rest, on the other hand, leads to collagen deconditioning, decreased tendon stiffness, and worsening symptoms over time.
Start with Isometrics: Early Pain Relief & Nervous System Reset
When tendons are cranky, movement can hurt, and that’s where isometric loading shines.
Williams and Gyer reference the well-known study by Rio et al. (2015), in which five 45-second isometric contractions at 70% of maximum voluntary contraction reduced patellar tendon pain for up to 45 minutes.
These contractions also reduced corticospinal inhibition, basically releasing the neural “brake” that often comes with tendon pain.
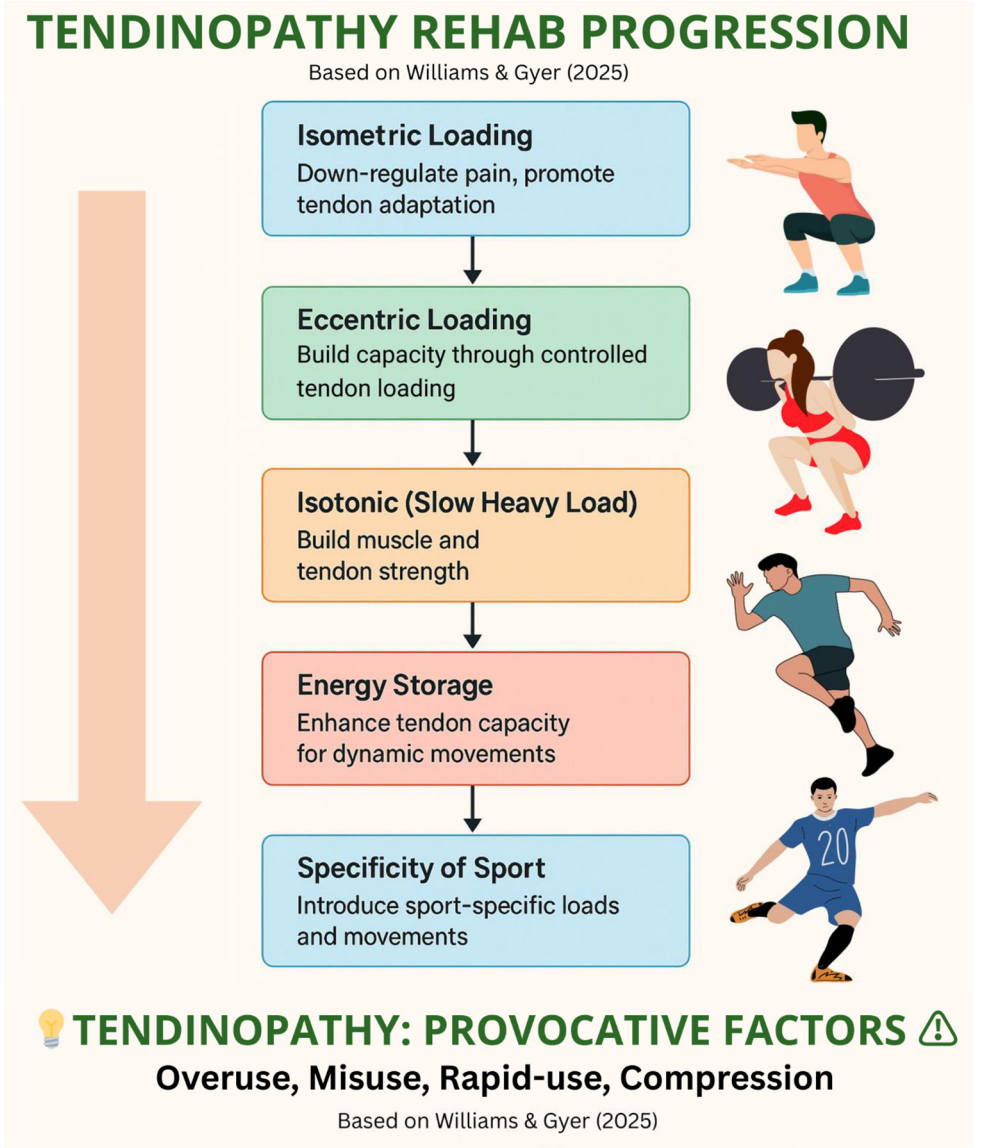
Rehab Progression: A Layered Approach
You don’t stop at isometrics. Here's the whole progression laid out in the paper:
- Isometric loading reduces pain and restores motor output
- Eccentric loading strengthens insertion points
- Isometric heavy slow loading improves structural capacity
- Energy storage & release to reintroduce elastic function (e.g., jumping, sprinting)
- Sport-specific loading and functional drills to reestablish readiness
This progression aligns with the tendon’s biology, providing a blueprint for both general and sport-specific rehabilitation.
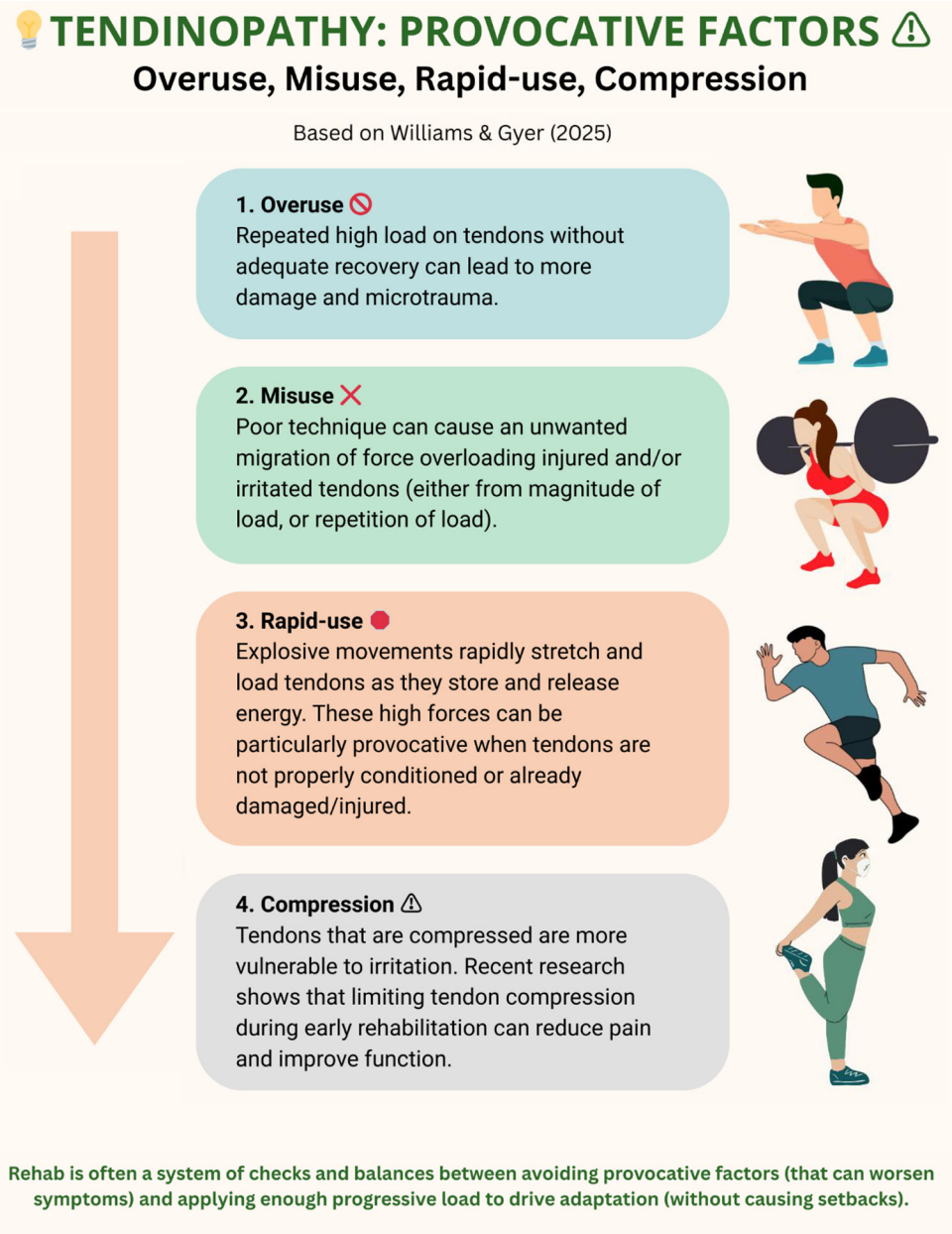
Tendon Provocation: Why Tendons Flare Up
Certain mechanical and training-related factors are more likely to trigger tendon pain and symptoms.
Understanding these concepts can help coaches and clinicians design more effective rehab and return-to-play progressions.
The four major contributors are:
Overuse
Repeated loading without sufficient recovery can lead to tendon breakdown, particularly in high-frequency training environments. Even submaximal loads, if applied too often, can exceed the tendon’s capacity.
Misuse
Poor movement quality or altered biomechanics (e.g., excessive valgus collapse or altered landing patterns) can distribute forces inefficiently, stressing the tendon in vulnerable ways.
Rapid Use
High-velocity or fast stretch-shortening cycle movements, such as sprinting, jumping, or abrupt decelerations, can trigger symptoms, particularly if reintroduced too soon in rehabilitation.
Compression
Certain joint angles or movements (e.g., deep knee flexion, dorsiflexion) increase compressive forces at the tendon’s insertion, which can irritate or overload already-sensitive tissue.
Train the Brain with TNT
Even after the tendon appears to be healed, athletes often struggle to move with full power and control.
That’s because the brain and nervous system may still be “holding back” due to pain or protective habits, like driving with one foot on the gas and the other on the brake.
This is where Tendon Neuroplastic Training (TNT) comes in.
TNT is a rehabilitation approach that specifically targets corticospinal excitability and inhibition, with the primary objective of maximizing rehabilitation and restoring full tendon function.
The use of metronome-paced strength training is a common approach in TNT.
Why? Research shows that this rhythm-based approach leads to better motor control and greater improvements in neural drive compared to self-paced lifting.
Pain Doesn’t Equal Damage
Here’s the tricky part: imaging doesn’t tell the whole story.
Research shows:
- Pathological tendons can be pain-free
- Painful tendons can appear normal on imaging
- Nerves often grow into tendons during degeneration, but not always in ways that map to pain
This means we can’t rely on MRI or ultrasound alone to guide rehab decisions.
Instead, we need to focus on function, specifically how the tendon moves, loads, performs, and recovers, rather than relying solely on imaging.
The goal in rehab isn’t to eliminate every bit of pain before loading; it’s to build back capacity and confidence through movement.
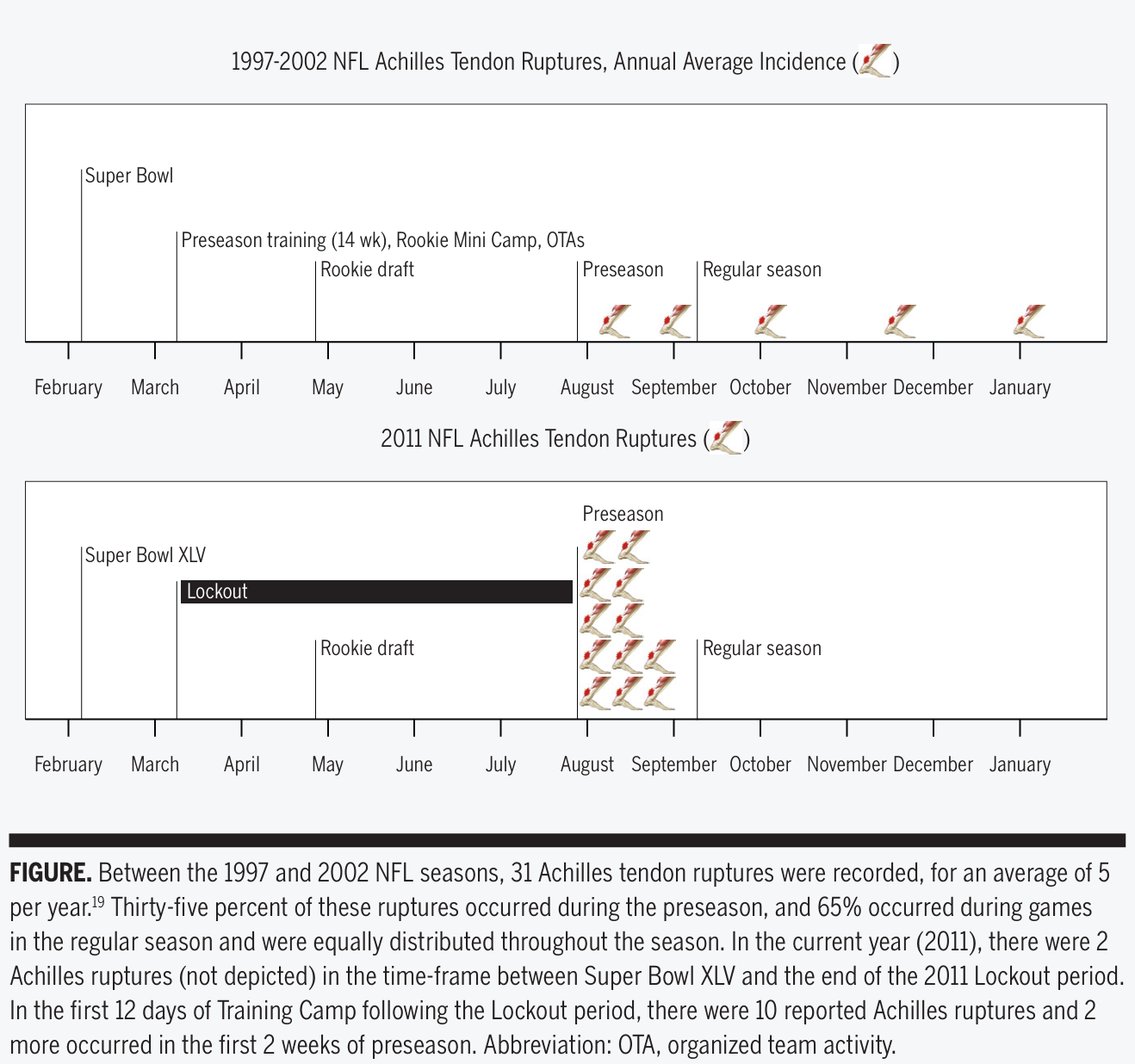
Case Study: The 2011 NFL Lockout
Unlike muscle, tendons have a low blood supply and a slower remodeling rate; therefore, they require long-term, progressive loading to develop stiffness, strength, and resilience.
When this process is skipped or rushed, the risk of injury skyrockets.
The 2011 NFL lockout was a perfect example of what happens when high loads are applied to unprepared tissue.
- During the 136-day lockout, players had no access to structured team training.
- When camps resumed, they went straight into high-intensity sessions with minimal prep.
- Result: 10 Achilles tendon ruptures in 12 days, compared to ~4 per full season.
This surge in tendon injuries, especially among rookies, highlighted what happens when high load meets low readiness.
No prep means no capacity, and proper loading protects the tendons.
Aging and Tendon Health: Still Adaptable, Just Slower
As we age, tendons undergo a series of cellular, structural, and functional changes that slow their ability to adapt, recover, and withstand mechanical stress.
Cellular Changes
- alters the shape and behavior of tendon cells (e.g., tenocytes), rendering them less effective in
- Aging also alters the shape and behavior of tendon cells (e.g., tenocytes), rendering them less effective in maintaining tendon integrity.
Structural & Mechanical Changes
- Tendon stiffness increases, while flexibility and resilience decrease.
- Cytoskeletal weakening and impaired collagen organization reduce the tendon's ability to respond to load and stress.
Metabolic Decline
- Older tendons produce less energy due to mitochondrial dysfunction.
- Protein synthesis slows down, limiting collagen repair and regeneration.
Slower Healing
- Fibroblasts divide more slowly.
- Key genes for tendon repair are downregulated.
- Cell-to-cell signaling is disrupted, impairing coordinated healing.
Coach's Takeaways
Tendinopathy isn’t just about inflammation.
It’s a complex condition rooted in how tendons respond (or fail to respond) to mechanical load.
Modern rehab should focus on:
- Progressive loading is the antidote, not the enemy.
- Isometrics are your best friend in the early stages.
- Progressively expose tendons to higher demands.
- Train motor control with intent and rhythm.
- Use function and response to guide rehab decisions.
- Manage load to prevent flare-ups and build resilience
Pain is complex. Load is the solution. Rehab is progression.,
I hope this helps,
Ramsey
Your Next Reads
- Tendon Basics: Effect of Mechanical Loading
- Tendon Healing Stages and Training Considerations
- Did the NFL Lockout Expose the Achilles Heel of Competitive Sports?
- Muscle vs. Tendon: Different Adaptations to Mechano-Metabolic Stimuli
Reference
Williams B, Gyer G. (2025). Tendons under load: Understanding pathology and progression. Journal of Musculoskeletal Surgery and Research.

